[difī,′,brilā,′,shə,n]
the termination of ventricular fibrillation or pulseless ventricular tachycardia (inefficient, asynchronous contraction) by delivery of an electric shock to the patient's precordium. It is a common emergency measure generally performed by a physician or specially trained nurse or paramedic. Defibrillation may be accomplished with defibrillator or special defibrillator pads. In external defibrillation, one paddle is placed to the right of the upper sternum below the clavicle, and the other is applied to the midaxillary line of the left lower rib cage. In internal defibrillation, which may be performed during open-heart surgery, the paddles are placed directly on the heart. The defibrillator, usually a condenser-discharge system, is set to deliver between 200 and 360 J. If shocks fail to restore a perfusion rhythm, cardiopulmonary resuscitation is begun. Repeat shocks also are attempted periodically until ventricular fibrillation ceases. defibrillate, v.
defibrillation[ de-fib&Prime,rĭ,-la´,shun ]
termination of atrial or ventricular fibrillation. usually by electric shock. Defibrillation by precordial shock is accomplished by delivering a nonsynchronized direct current to the myocardium. It is an emergency procedure, used to terminate a life-threatening ventricular arrhythmia. The electric shock is delivered either by placing metal paddles on the chest (closed defibrillation ) or by applying paddles directly to the heart muscle, as in cardiac surgery.
The high-voltage electrical current delivered during precordial shock causes complete depolarization of the heart muscle, disrupting all of the electrical circuits that are activating the heart muscle and causing ventricular fibrillation. This allows the heart's natural pacemaker to regain control and regulation of the heart rate and rhythm.
The procedure carries some risk and should be done only by specially trained physicians, nurses, and paramedics. Cardiopulmonary resuscitation and the administration of intravenous fluids and drugs are essential components of defibrillation. Sodium bicarbonate is given to combat acidosis, lidocaine or amiodarone is given to forestall arrhythmias that may develop during and after defibrillation.
Electrocardiographic readings and assessment of ECG patterns are done prior to the procedure to verify the presence of a lethal arrhythmia, and afterwards to evaluate the effectiveness of the treatment. Some ECG machines and cardiac monitors can continue to function during defibrillation because they have been designed to withstand the electrical shock when it is delivered to the patient.
Burns of the skin may occur under the paddles at the time of defibrillation, steroid or lanolin-based ointments or creams are usually prescribed as treatment. The use of conduction gel and close contact of paddles to skin may prevent burns. More serious complications of defibrillation include cardiac arrest, respiratory arrest, neurologic impairment, pulmonary edema, and pulmonary and systemic emboli. The patient must be monitored carefully after the procedure for return of ventricular fibrillation. Additional observations include changes in blood pressure, pulse rate, rhythm, and character, state of consciousness, and adequacy of ventilation.
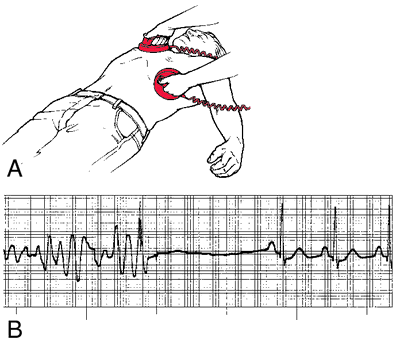
&emsp,Defibrillation: A, Anterolateral paddle placement for external countershock. External paddles are placed at the second right intercostal space and at the anterior axillary line in the fifth left intercostal space. B, Ventricular fibrillation converted to normal sinus rhythm with external countershock. From Polaski and Tatro, 1996.






0 comments:
Post a Comment