As of 2010, holders of a CHPN (Certified Hospice and Palliative Nurse) certificate may renew their certificates in two ways. The first way is to successfully pass the computer-based examination in March, June, September, or November of the year in which their certificate expires. The second way is to complete the alternative method of renewal, which is to accumulate points through a variety of professional development activities.
For those interested in taking the computer-based examination, the following information will be helpful.
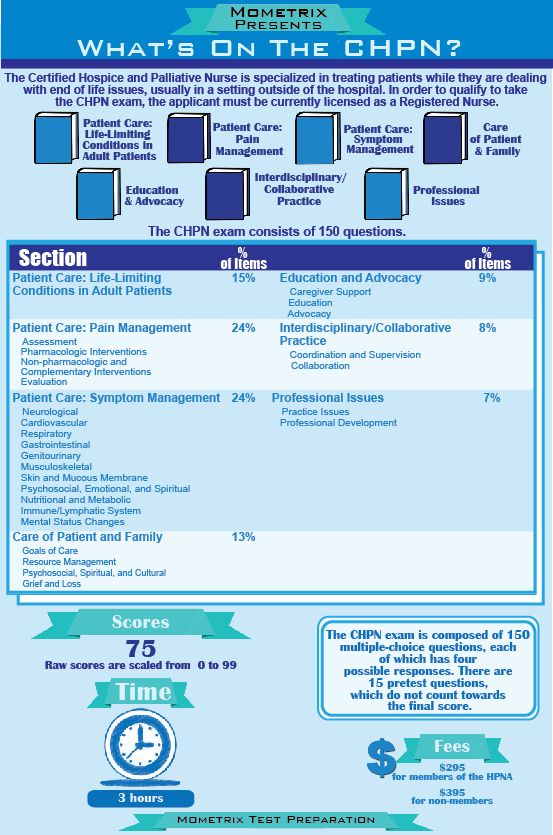
The Certification Examination for Hospice and Palliative Nurses is made up of 150 multiple-choice questions, 135 of which are scored and 15 of which comprise a non-scored pre-test. Each CHPN exam question has four response alternatives (A, B, C, and D), one of which represents the correct answer. For a candidate to be awarded the CHPN credential, he or she must complete the CHPN exam within three hours and achieve a passing score.
The examination is prepared by the NBCHPN (National Board for Certification of Hospice and Palliative Nurses). Individuals who have expertise in hospice and palliative care write the questions and evaluate them on the basis of relevance, consistency, accuracy, and appropriateness.
Before the test application deadline, the candidate for CHPN certification must hold a current, unrestricted registered nurse license in the United States, its territories, or the equivalent Canadian license. In addition, the NBCHPN recommends (but does not require) at least two years of experience in hospice and palliative nursing practice. The reason for this is that the examination questions are based on what a nurse normally learns during two years of practice in end-of-life care. Therefore, persons with less than two years' experience may have difficulty passing the examination. However, recognizing that individuals learn at different rates and through different methods, the NBCHPN will allow any licensed registered nurse who considers himself or herself to be ready to take the examination.
The content of the CHPN exam is based on the activities performed by hospice and palliative nurses involved in end-of-life care. CHPN exam candidates should be prepared for the following types of questions:- Recall: About 30 percent of the questions require that the candidate recall or recognize specific information.
- Application: About 50 percent of the questions require the ability to understand, relate, or apply knowledge to new or changing situations.
- Analysis: About 20 percent of the questions require the ability to analyze and synthesize information, determine solutions, or evaluate the effectiveness of a solution.
1. After the history, physical examination, and urinalysis, a useful initial tool in assessing urinary incontinence in the palliative care patient is:
- Urodynamic testing
- A multiday bladder log
- Spinal magnetic resonance imaging
- A trial of systemic hormone replacement therapy
2. If an adult patient is concerned about the emotional effect of his terminal illness on his 7-year-old child, the hospice nurse should explain that:
- A 7-year-old child is not old enough to understand serious illness and death
- Changing family routines will help the child come to terms with the illness
- There are age-appropriate ways to assist a child through the grieving process
- It is helpful to let the child overhear other family members talking about the death of the parent rather than having a direct conversation
3. A benefit of using a pain assessment tool (e.g. pain scale) in the palliative care patient is the ability to:
- Observe a trend in the patient's response to analgesic therapy
- Treat the adverse effects of pain medications
- Detect symptoms of drug withdrawal
- Differentiate true pain from drug-seeking behavior
4. Patients with acquired immunodeficiency syndrome most commonly die as a result of:
- Malignancy
- Heart failure
- Opportunistic infections
- Renal failure
5. A terminally ill patient is showing decreased awareness of his surroundings, decreased oral intake of solids or liquids, and is no longer able to get out of bed. The most likely explanation for this constellation of findings is:
- Loss of hope
- Impending death
- Depression
- Urinary retention
1. B: Urinary incontinence is a common symptom in the palliative care patient and may significantly affect a patient's self-esteem, sexual activity, and willingness to venture out in his or her community. There are multiple causes of urinary incontinence, including urinary tract infections, limited mobility, affecting a patient's ability to get to a toilet, constipation, mental status changes, medication effects, weak pelvic floor musculature, neuropathic bladder, fistula, and poor urethral sphincter tone. Management of urinary incontinence varies greatly, depending on the cause. A patient with invasive prostate cancer, causing incontinence, needs treatment strategies that differ from those needed by a patient with a urinary tract infection. A thorough history, including a medication history, physical examination, and urinalysis often reveals likely etiologies of urinary incontinence. Additionally, a bladder log, which details fluid intake, voiding, incontinence episodes, and any associated factors (e.g. coughing, laughing) can be helpful in designing a management plan.
2. C: Palliative patients who have young children are often very concerned about the effect their death will have on their children. Helping a patient and his or her family feel more comfortable with assisting the children through the dying and grieving process can bring a patient a great deal of comfort. A child's understanding of illness and death and the way in which their grief is expressed often varies greatly, depending on their age and development. Many adults mistakenly believe that a young child is either unaware of the parent's illness or is unable to understand the severity of a parent's illness. Many families need and desire specific, concrete strategies for explaining the illness and death of a parent to a child. Maintaining as many of the child's usual routines as possible, answering questions directly, and encouraging the child to express any thoughts or feelings are among the helpful tips that families may need.
3. A: Pain assessment is a crucial part of palliative care nursing, and there are many different assessment tools available to the palliative care nurse for this purpose. Although not universal, pain is an extremely common symptom in the dying patient. Pain is far more than a purely physical experience for the patient, and the most effective assessment tools take into account the multiple factors that influence the individual patient's pain experience. Important factors to assess (and reassess) include specific words describing the pain, intensity (e.g. 1-10 scale), location, duration, quality, associated factors, effect on sleep, appetite, mood, and energy, and the patient's attitudes or beliefs about his or her pain. Using a consistent assessment tool allows the nurse to observe trends in the patient's pain in response to therapy. Although a multifactorial assessment tool may discover adverse medication effects, withdrawal symptoms, or warning signs of psychological dependence on pain medications, most pain assessment tools are not designed for the primary assessment of these issues.
4. C: Acquired immunodeficiency syndrome (AIDS) is caused by human immunodeficiency virus (HIV), a retrovirus that primarily affects the T-cells of the human immune system. T-cells carry a surface protein called CD4, and the disease severity correlates with falling CD4 levels. Although the discovery and use of antiretroviral medications have markedly changed the life expectancy of most patients with HIV/AIDS, it remains a fatal illness. Because HIV affects the patient's immune system, progression of disease is primarily characterized by opportunistic infections (i.e. infections that would not occur in a patient with healthy T-cells). AIDS patients may also develop opportunistic malignancies, such as Kaposi's sarcoma and lymphoma, although infection is the primary cause of death in AIDS patients. Examples of opportunistic infections that occur as CD4 levels decrease include pneumocystis carinii, tuberculosis, and cryptococcus. Aside from the effects of infections, AIDS patients often require end-of-life care for pain, weight loss, weakness, and mental status changes.
5. B: Although each patient's dying process is individual, the signs and symptoms of impending death are often very similar, even in patients with very different terminal illnesses. The palliative care nurse should be familiar with the common signs and symptoms of impending death so that he or she can educate the patient and caregivers about the dying process and support patients and caregivers through the patient's death. As death nears, the patient has decreasing interest in or awareness of his or her surroundings and a reduced desire or ability to move around. He or she has a marked decrease in food or fluid intake and often develops difficulty with swallowing. The dying patient usually develops noisy and irregular respirations, cool extremities, and the pulse may become fast or irregular. Urine output typically decreases or stops as the patient gets closer to dying.






0 comments:
Post a Comment